
If you have kids, or have been around any kids, you know that vomiting happens. Gastroenteritis is common, and usually a benign illness. But when is vomiting more than just gastro? This PEM4 series of cases will highlight some of the vomiting Red Flags in infants and diagnosis.
It's all about the age
Like most things in Pediatrics, the age of the patient matters. Depending on the patient’s age, your differential diagnosis will change. Some disease processes are more common in the younger patients than the older. As a general rule, the younger the patient with vomiting, the more concerned you should be.
For example, let’s take a 2 year old and a 2 week old with vomiting and poor intake. These are two patients with the same history, but could have very different pathology! A 2 week old has very few responsibilities in life– eat, pee, poop, sleep. As a general rule, if one of those isn’t going well, be concerned. The 2 year old however, who maybe tolerates a popsicle a few times during the day, is a lot more reassuring.
Case 1
A 5 week old male presents from the pediatrician office with dehydration. Mom reports patient has been spitting up feeds, which had been attributed to reflux on her prior visit earlier in the week, but today she was sent to the ED because it was noted that he had weight loss from his last pediatrician appointment.
His vital signs when you see him include a Temp of 36.1C HR 151 BP 88/76 RR 18 SpO2 100%
On your exam, he is lethargic and very thin appearing. His anterior fontanelle is sunken and his lips look dry. His abdomen is not distended, not tender and soft to palpation.
Certainly, the vital signs and exam of this child are concerning. There is also a clue in the history– the weight loss. RED FLAG! Weight loss in a child should always be worrisome, but especially for a 5 week old!
You decide to obtain labwork, seen here.
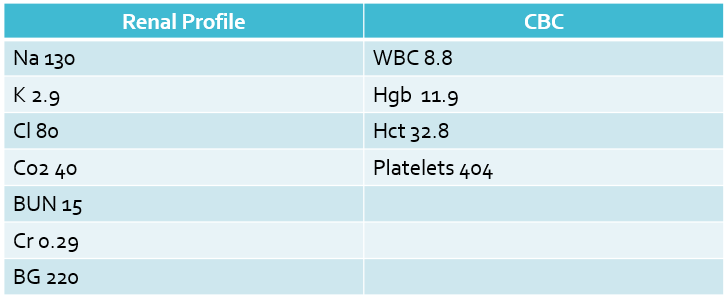
The patient has hyponatremia, with a hypochloremic, hypokalemic metabolic alkalosis.
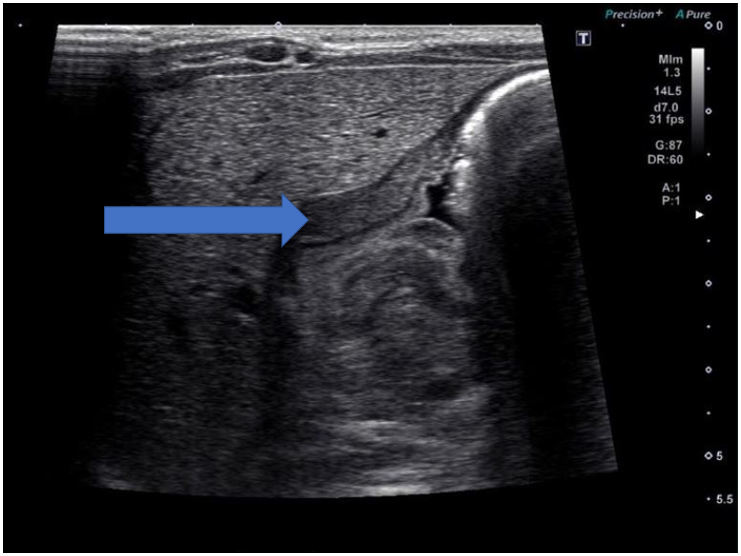
Ultrasound!
An ultrasound of the pylorus was obtained.
An easy way to remember if the pylorus is thickened or not is “Pi”lorus or 3.14. If the thickness of the pylorus is >3mm and >14mm in length, it is likely hypertrophic pyloric stenosis.
Hypertrophic Pyloric Stenosis
Classic presentation is a first born male at 3-6 weeks of age. The textbook history state there is “projectile” NBNB vomiting, through this history is difficult to obtain (many parents will describe any vomiting as “projectile”).
Classic lab findings are hypochloremic, hypokalemic metabolic acidosis, as seen in this case. Infants often are presenting earlier with increasing availability of ultrasound, so these lab abnormalities may not be seen. Ultrasound will show a thickened pylorus– remember your “Pi” mnemonic as described above.
Treatment is usually surgical correction.
References
Fleisher, G. R., & Ludwig, S. (Eds.). (2016). Textbook of pediatric emergency medicine. 7th Edition. Lippincott Williams & Wilkins.
Parashette, K & Croffie, J. (2013). Vomiting. Pediatrics in review, 34(7), 307-321.
Patel, R et al. Infantile hypertropic pyloric stenosis (IHPS): it can take away your breath, alertness, wee and poo. BMJ Case Rep. 2013. Published online 2013 Nov 20. doi:[10.1136/bcr-2013-201435
Sivitz, Adam B., Cena Tejani, and Stephanie G. Cohen. “Evaluation of hypertrophic pyloric stenosis by pediatric emergency physician sonography.”Academic Emergency Medicine 20.7 (2013): 646-651.

Katie Edmunds is a current Pediatric Emergency Medicine Fellow interested in creating PEM 4 all those who are given the responsibility of treating the sickest babies wherever they may be.

