In the Pediatric Emergency Department, the first few minutes of a cardiac arrest can be a blur. Anxious EMS providers are bringing in a critically ill child and transitioning care to the ED team who are trying to take over. You, the physician, the team leader, are trying to juggle all the information flying at you. This PEM4 To The POINT post aims to share one (of likely many) ways that we as team leaders can approach the initial few minutes of a pediatric cardiac arrest.
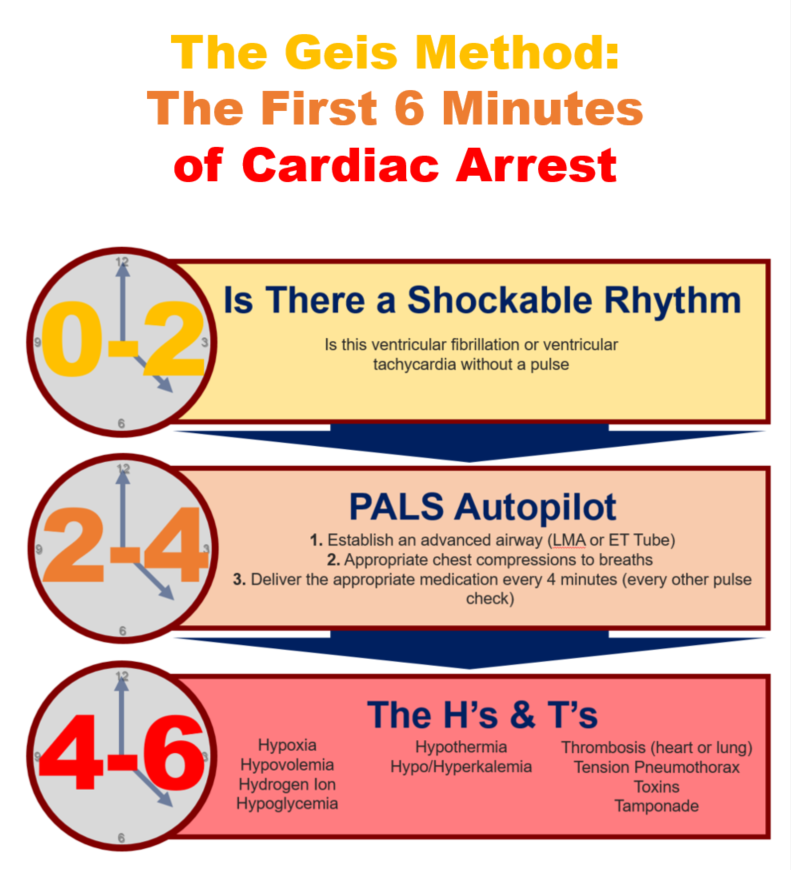
0 - 2 Minutes: The Transition and Shock or Not
The initial moments of taking over the management of a child in cardiac arrest are critical. Hopefully, there is some time to prepare and place the CPR backboard, draw up estimated weight based doses of epinephrine, and have the defibrillator ready. The most important question you need to answer in the first 2 minutes of the patients arrival:
Is there a shockable rhythm?
The team needs to answer that question as soon as possible. If the rhythm is ventricular tachycardia or ventricular fibrillation, deliver an appropriate shock. We know that delay in defibrillation leads to increased mortality and decrease the chances of survival to discharge [1]. The key steps in determining the answer to this question is getting the defibrillator pads on the patient and assessing the rhythm. If there is time prior to the patient’s arrival, discuss with the team how that will occur during the transition of care from the EMS providers, all while preventing time off the chest during compressions.
2 - 4 Minutes: PALS Autopilot
The goal of the next few minutes is to have your team performing good CPR on autopilot so the cognitive burden is off of you as the team leader. In order to do this, you need to make sure a few things are happening.
1. Establish an advanced airway (LMA or ET Tube)
2. Appropriate chest compressions to breaths
3. Deliver the appropriate medication every 4 minutes (every other pulse check)
Make sure that each of these things is being done well and will occur without prompting from the team leader. A CPR coach can support the compressions, the recorder can let the team know when an epinephrine dose is needed, and the airway manager can provide good ventilatory breaths. By putting PALS autopilot, a huge cognitive burden is taken off the team leader, leaving them to work on the next 2 minutes.
4 - 6 Minutes: The H's and T's
Now that the team has determined if a shock is needed and excellent CPR is occurring, the team leader can run through and address the reversible causes of arrest.
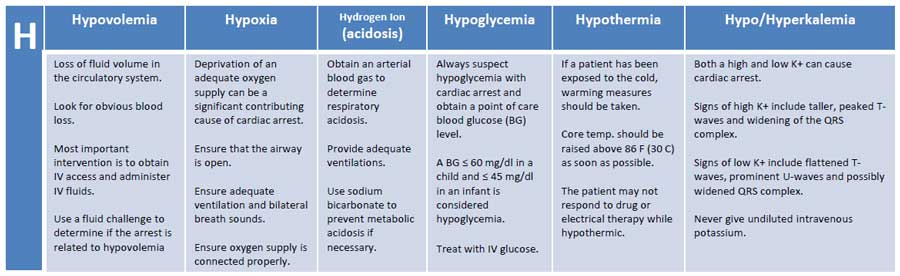
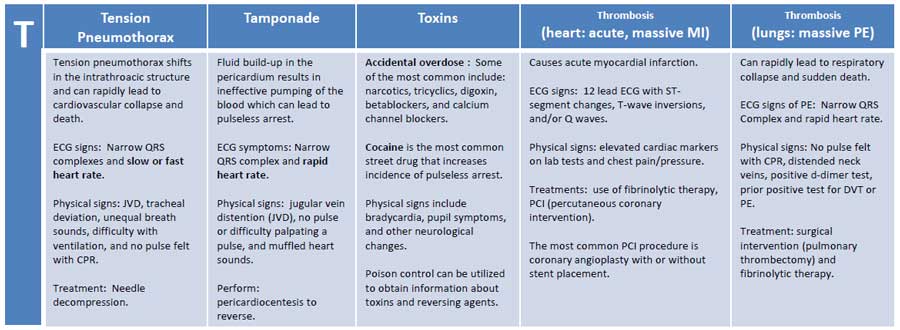
The H’s and T’s
With the final 2 minutes, identify and address the H’s and T’s through labs and bedside imaging.
Method to the Madness
Thanks to Dr. Gary Geis, MD from Cincinnati Children’s Hospital Medical Center for teaching me this. This is just one method on how to control the mental burden and the stress of managing a child in cardiac arrest and by no means is it the only or even the best way. The main learning point is to develop SOME method to standardize the first few minutes. Similar to ATLS, by sticking with an algorithm, things aren’t forgotten.


Ashish Shah is an assistant professor and Pediatrics and Family Medicine Residency Education Director at Rady Children’s Hospital interested in creating PEM 4 all stages of learners caring for children seen in the emergency department