Welcome to this addition of PEM Core. We’re going to delve into the topic of vasopressors in the pediatric emergency department. We were lucky enough to have Dr. Matt Zackoff (@MZackoff) give a PEM focused talk on how to think about vasopressor choice. Sit back and relax as we try to take the pressure off pressure choice.
What is Shock?
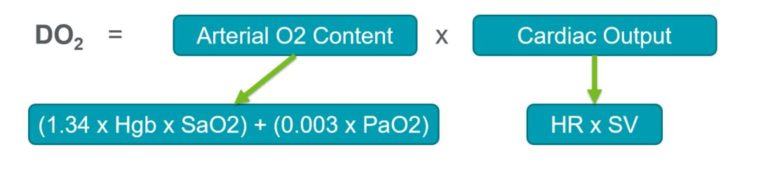
At its core, shock is when oxygen delivery (DO2) fails to meet tissue metabolic demand (VO2). As physicians, we attempt to augment our patient’s DO2 as much as possible in hopes to support the body in meeting that metabolic demand during their shock state.
When DO2 fails to meet VO2, the system starts to fail. The body attempts to support that imbalance by changing the cardiac output and the arterial O2 content.
(For the sake of this post, we won’t be digging into the ways to augment oxygen content delivery).
Cardiac Output
We attempt to evaluate and augment the cardiac output in the emergency department regularly.
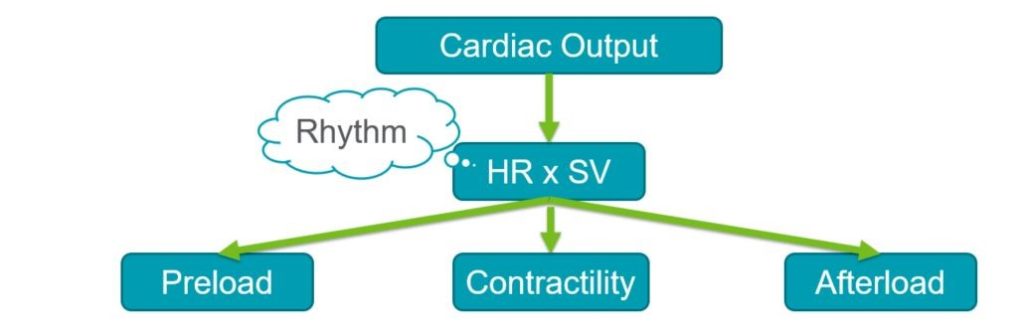
When determining his patient’s cardiac output, Dr. Zackoff asks himself a few questions:
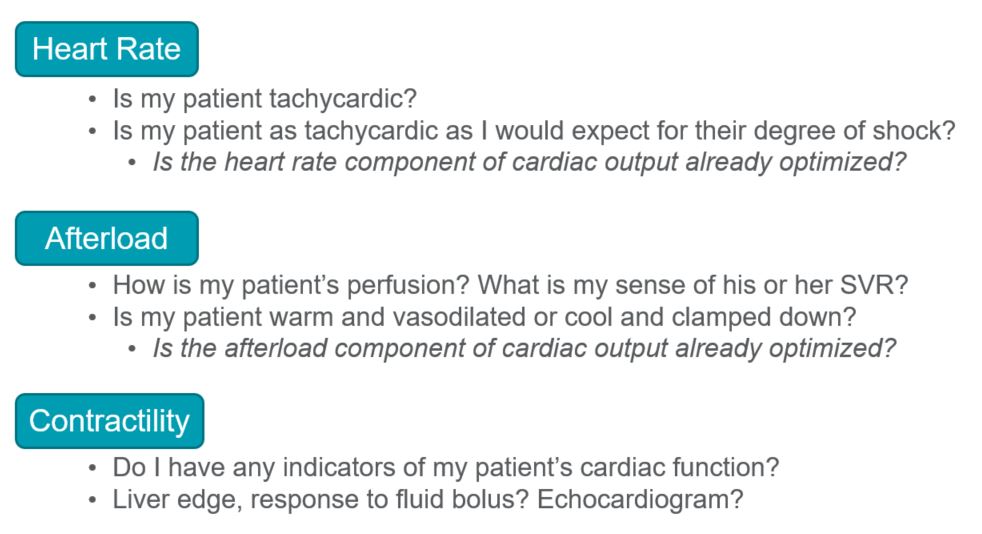
We can easily obtain a heart rate (HR) through our initial monitoring. Determining the preload, contractility, and afterload (systemic vascular resistance) is more difficult without more invasive measure. However, using the physical exam (capillary refill, pulse quality, skin assessment, mental status) blood pressure (MAP), and POCUS, we can get a better idea of the physiology. And with that understanding, decide on the best plan of action.
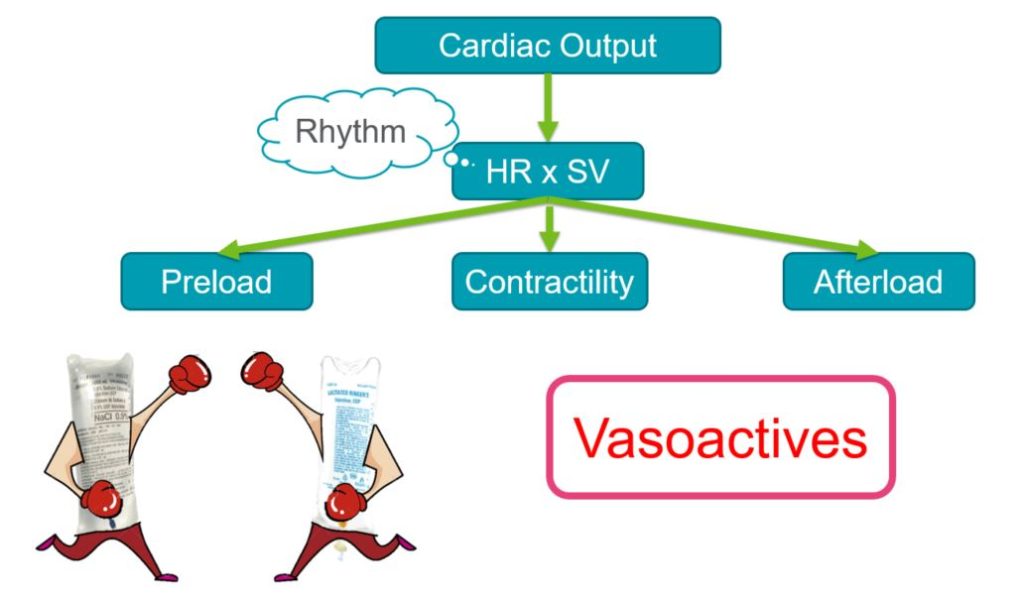
The Goldilocks Vasopressor
Before picking the ideal vasopressor, you must ask the questions listed above. This will give you a better understanding of the underlying physiology of the patient and attempt to categorize them as Cold Shock (high SVR state) or Warm Shock (low SVR state), and thus guide your vasopressor choice.
Below is a list of vasopressors. The two most commonly used in our emergency department are epinephrine and norepinephrine. Some may be more available than others at your institution.
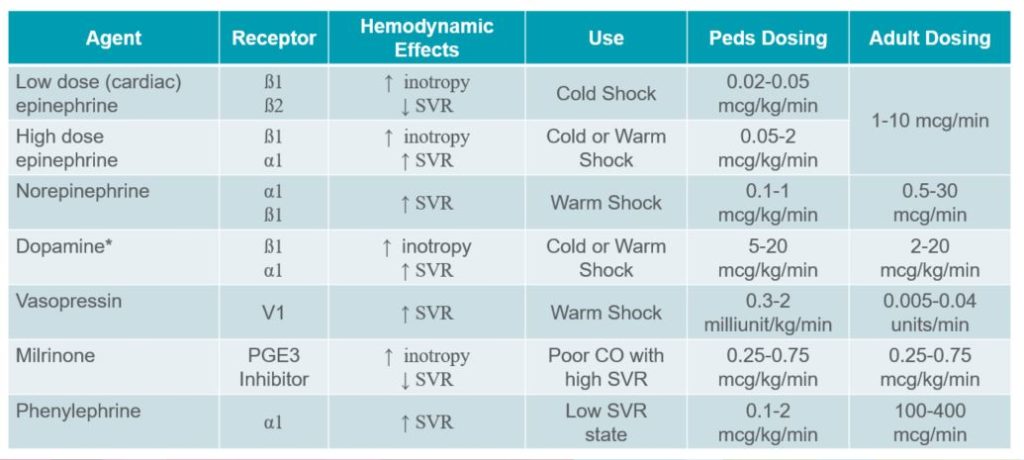
*Dopamine is being used less and less with better and more predictable choices.
Another choice that is particularly useful in the neonate and infant population is a Calcium infusion (5-10mcg/kg/hr). Infants and neonates have low total body levels of calcium which quickly become depleted.
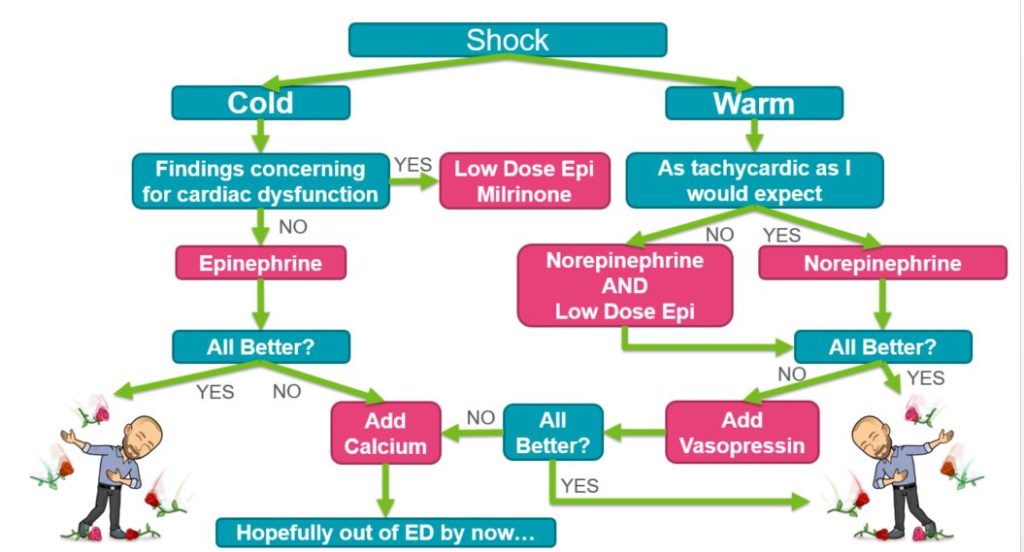
The Zackoff Method
Not yet trademarked. Dr. Zackoff puts it all together in this algorithm on how he thinks about vasopressor choice in the emergency department. He emphasizes that the choice should be based on the patient’s physiology and that adjustments can and should be made based on patient response.
(This is just one of many ways to think about vasopressor choice)
All images used with permission from Dr. Zackoff.

Dr. Zackoff MD, MEd is a board certified Pediatric Critical Care Physician at Cincinnati Children’s Hospital Medical Center. He has an interest in education and using novel technologies (Augmented Reality, Virtual Reality, Mixed Reality) to improve care at the bedside.
Follow him on twitter @MZackoff



