Getting the notification of an incoming full arrest is one of the most adrenaline inducing moments in the pediatric emergency department. Annually, >5000 children will have an out-of-hospital cardiac arrest. Of those arrests, we achieve return of spontaneous circulation (ROSC) on ~36% of those cases with overall reported survival between 6.4%-10.2%. The most amazing part, up to 77% have favorable neurological outcomes!!!
In August 2019, the American Heart Association came out with a Scientific Statement on the best practice on pediatric post-cardiac arrest care. This was a DENSE but important article and I implore you to read it as this post will not go into all of the evidence the authors used to make their recommendations. This post is an attempt to condense their recommendations focusing on what we can do as PEM physicians in the emergency department.
General Principals
Patients experience post-cardiac arrest syndrome (PCAS) from the moment ROSC is achieved through discharge. Below is a figure showing the timeline of PCAS with the overall goal of care being prevention of recurrence of arrest and limiting further injury following ROSC. Where we as emergency medicine providers can optimize care for our patients is in the Immediate and Early Phases of PCAS.
Post-Cardiac Arrest Syndrome Timeline
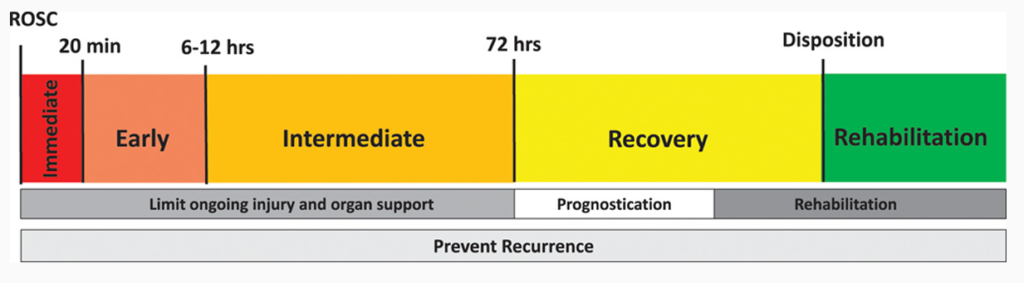
Image taken from Topjian et al article on Pediatric Post-Cardiac Arrest Care. Times are not hard a fast and can vary from patient to patient.
Limiting Further Injury
In the Immediate and Early Phase of PCAS, providers should optimize their care to prevent further injury to the body after the arrest. A solid understanding of the pathophysiology of the four major components of PCAS are essential to the prevention of further injury. These four components are post-cardiac arrest brain injury, post-cardiac arrest myocardial dysfunction, systemic ischemia/reperfusion response and the underlying precipitating pathology that led to the arrest.
Post-Cardiac Arrest Brain Injury
Post-cardiac arrest brain injury is the leading cause of morbidity and mortality in ROSC pediatric patients. In addition, the other three factors that influence PCAS can lead to worsening brain injury as well. The major culprits are direct hypoxemic and hypotensive injury from energy deprivation during the cardiac arrest. However, the sudden ROSC also leads to an abrupt rush of free radical oxydative stress furthering the neurological injury. What does that all mean? Well, it means that hypoxemia and hypotension are bad (duh) but it also means that hyperoxia and a goal of 100% SpO2 may also be harmful.
Clinical Manifestation of Post-Cardiac Brain Injury:
Cerebral edema, seizures, myoclonic jerks, autonomic dysfunction, coma, seizures, and long-term neruobehavioral dysfunction.
Post-Cardiac Arrest Myocardial Dysfunction
Myocardial stunning after an arrest leads to the post-cardiac arrest myocardial dysfunction. Due to the absence of flow during arrest, cardiac dysfunction in inevitable. The onset is directly after ROSC, peaks within ~8hrs. Function generally improves over the next few days and resolves in 2-3 days. For providers in the ED, we will always have to keep this in mind when managing ROSC patients with PCAS. It does not occur in all patients and the pathophysiology is not entirely understood. What is known is that it occurs in approximately 2/3rd of patients, and ischemia/reperfusion injury, and catecholamine and cytokine mediated myocardial injury are both thought to play a part. Because this is something that generally improves with time, we as providers may be able to modify this factor.
Clinical Manifestation of Post-Cardiac Myocardial Dysfunction:
Hypotension, arrhythmias, LV or RV dysfunction (diastolic or systolic), decreased cardiac output, pulmonary edema, recurrence of cardiac arrest.
Systemic Ischemia/Reperfusion Response
Similar to sepsis, the injuries caused by the systemic ischemia/reperfusion response revolves around cytokines and endotoxins in the plasma, unregulated activation of the coagulation pathways, and inhibition of the anticoagulant pathways. With the patient experiencing a sudden change from a no-flow/low-flow state where cell injury and cytokine leak is occurring, to an imporved flow post cardiac arrest, mobilization and flow of those molecules to organs leads to injury.
Clinical Manifestation of Systemic Ischemia/Reperfusion Response:
Capillary leak, DIC, coagulopathy, adrenal insufficiency, multisystem organ failure, hyperglycemia, intravascular hypovolemia, low systemic vascular resistance (vasoplegia).
Underlying Precipitating Pathology
An often overlooked component of ROSC management is identifying and managing the initial insult that led to the arrest. For example, if it is an arrest caused by sepsis, starting antibiotics and aggressive cardiovascular support will be important to prevent recurrence of cardiac arrest. Another example is hyperkalemia induced cardiac arrest. Without decreasing the potassium, subsequent arrest may be unavoidable.
Clinical Manifestation of Precipitating Pathology:
Can vary significantly based on the cause of arrest. Be judicious in completing a systematic investigation to identify the cause of arrest– ie the H’s and T’s (shown below)
The H's & T's
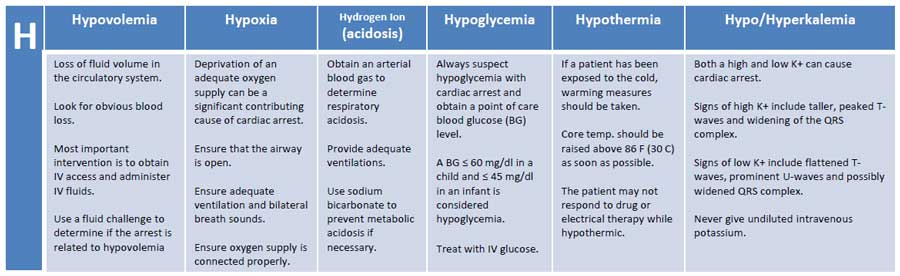
H’s and T’s with methods of identification. Image taken from Learn and Master ACLS/PALS.
Monitoring & Therapeutic Strategies in the Emergency Department
Much of the post-cardiac arrest care is going to happen in the Pediatric Intensive Care Unit. Instead of going in depth into the strategies that occur in the ICU, we will look at what we as emergency department providers can do in the Immediate and Early Phases of managing PCAS.
Immediate and Early Phase Monitoring
At minimum, children receiving post-cardiac arrest care should have these non-invasive monitors, imaging, and labs completed:
Pulse Oximetry
EtCO2 Capnography
Cardiac Telemetry
Arterial/Venous Blood Gas
Coagulation Studies
+/- CXR
Blood Pressure Monitoring
Continuous Temperature Monitoring
Continuous Urine Output
Electrolytes
Blood Glucose
+/- CT Scan (if traumatic arrest)
Other monitoring such as continuous EEG, echocardiography, CT/MRI Brain, central venous catheters, arterial catheters will likely be initiated in the ICU setting but can be started in the ED based on physician comfort with the procedures.
Therapeutic Strategies: Blood Pressure and Circulatory Support
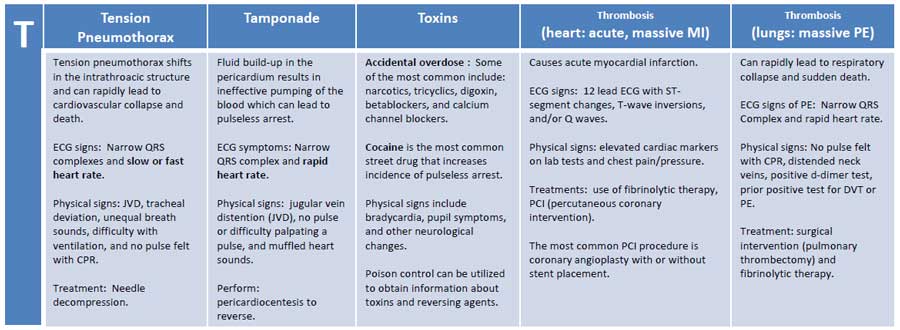
Hypotension during the Immediate Phase of PCAS is a known risk factor that decreases survival to discharge from the hospital. As Emergency Medicine providers, it is essential we provide immediate blood pressure support. What is most concerning is that in the Therapeutic Hypothermia After Pediatric Cardiac Arrest of OHCA (THAPCA-OH), only 41% of children received vasopressor support for their hypotension following ROSC. We need to do better. Although the evidence is not causal when it comes to hypotension and outcomes, setting blood pressure goals early and reaching those goals through the administration of IV fluids and vasopressors makes sense. The recommendation from the Topijan et al article is to maintain a blood pressure greater than the 5th %ile for age. Unfortunately, there is no available evidence that helps delineate when to give IV fluids and when to start vasopressor therapy (Table 2).
Therapeutic Strategies: Arrhythmia Control
Arrhythmia is a complication that can occur following ROSC and may also be the inciting event that caused the arrest in the first place. There is not enough evidence for the authors of the statement to recommend giving prophylactic anti-arrhythmics and instead, anti-arrhythmic therapies should be selected on an individual case basis. If there is uncertainty, obtaining and EKG and consulting with a pediatric cardiologist is likely the best course of action. Be aware that many of the vasoactive medications that we use regularly are arrhythmogenic and may precipitate an arrhythmia.
Therapeutic Strategies: Oxygenation
During cardiac arrest we put our patients on 100% FiO2 trying to get as much oxygen to the organs as possible. In the no-flow state of arrest, this is essential. After ROSC, as we talked about above, hyperoxia AND/OR hypoxemia both were found to increase mortality in the limited evidence available. Ideally, an arterial blood gas can be obtained relatively quickly after ROSC and can be used to help guide FiO2. The authors recommend shooting for a PaO2 level between 60-300 mmHg OR maintaining an oxygen saturation between 94%-99%.
Therapeutic Strategies: Ventilation
End Tidal CO2 capnometry monitoring is a great non-invasive way to estimate the PaCO2 in the blood stream and at the alveoli. Over on the adult side, the International Liaison Committee on Resuscitation recommends using EtCO2 during arrest as it is a surrogate for cardiac output. It is not as well studied on the pediatric side but the authors of the statement recommend its use during arrest and in the PCAS period. They recommend targeting normocapnia (PaCO2 35-45 mmHg). After correlating the PaCO2 with the EtCO2, providers can adjust based on the EtCO2 reading.
Therapeutic Strategies: Temperature Management
The Therapeutic Hypothermia After Pediatric Cardiac Arrest of OHCA (THAPCA-OH) study which looked at targeted temperature management (ie therapeutic hypothermia vs normothermia) and it effect on neurological outcomes at 1 year found no significant difference between the two groups. What has shown to lead to poor outcomes is hyperthermia after ROSC. With that in mind, if your institution does not have a protocol in place for theraputic hypothermia, the authors recommend setting temperature goal between 36-37.5 Celsius.
Therapeutic Strategies: Seizures and ECMO
Seizures are a common occurrence and can effect up to 50% of children after ROSC. Most seizures are subclinical and will require an EEG in the ICU to discover. In the emergency department, if there are overt signs of clinical seizure activity, the authors recommend weighing the risk of treatment with hemodynamic status.
Be aware of your institutions ECMO protocols and guidelines to determine if the child in front of you is a candidate. ECMO can be used both in the PCAS period and during CPR via ECPR. There are no solid guidelines in the literature on who is a candidate for ECMO in OHCA pediatric cases.
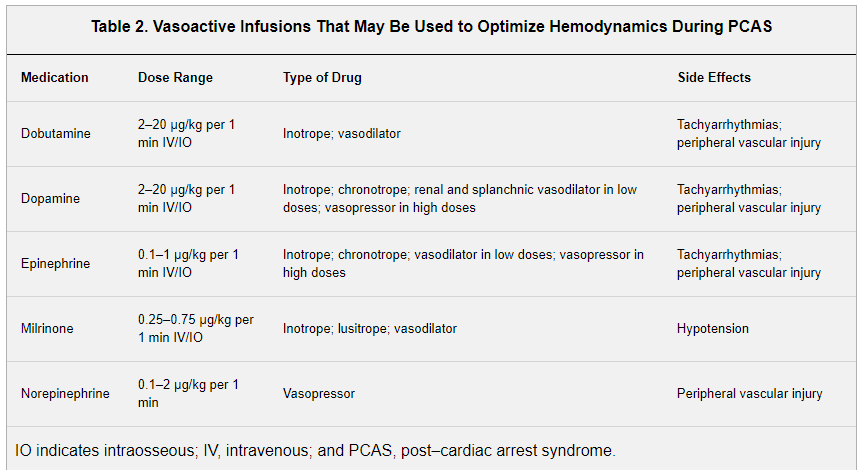
The Whole Package
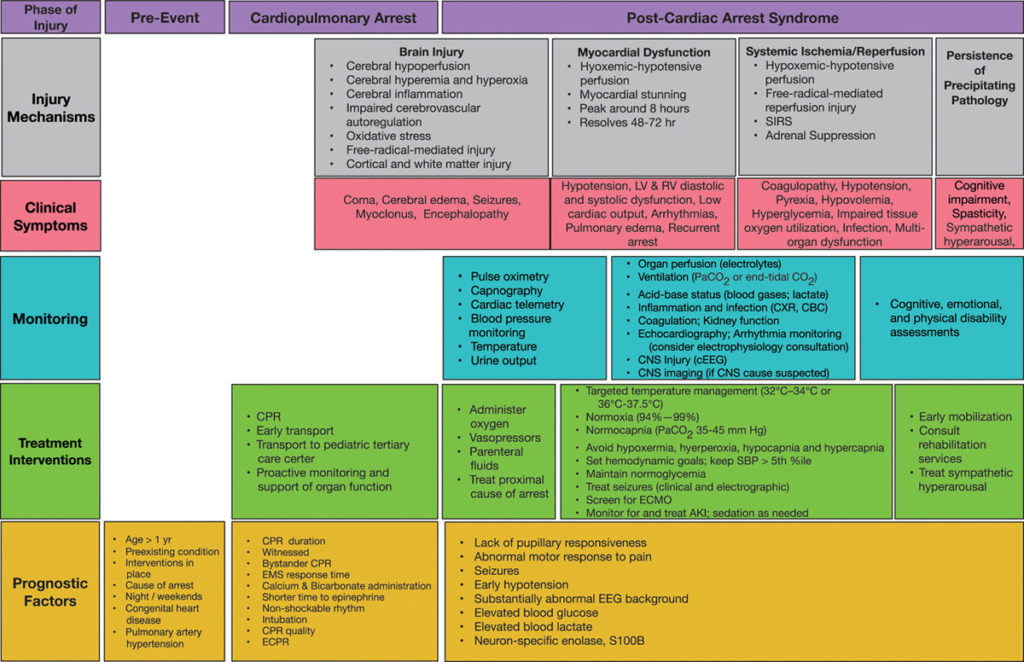
Image taken from Topjian et al article on Pediatric Post-Cardiac Arrest Care. An awesome infograph showing the pathophysiology with the optimal management recommendations.

1. When it comes to targeted Oxygenation, Ventilation, and Temperature, go for the “Goldilocks Zone”
Normoxia (94%-99% SpO2 or PaO2 60-300 mmHg)
Normocapnea (PaCO2 35-45 mmHG)
Normothermia (36-37.5 C)
2. Try to limit further injury by watching for clinical manifestations of brain injury, myocardial dysfunction, and systemic hypoperfusion/reperfusion response.
3. Maintain a blood pressure >5th percentile for age following ROSC through IV Fluids and Vasopressors.
4. Manage the underlying precipitating pathology (H’s & T’s).
5. Just read the whole Statement for yourself.
References

Ashish Shah is an assistant professor and Pediatrics and Family Medicine Residency Education Director at Rady Children’s Hospital interested in creating PEM 4 all stages of learners caring for children seen in the emergency department




