PEM Core is a monthly curriculum focused on reviewing PEM Certification Exam (Boards) Content. It is not intended to be a complete review of a case, but rather to “hit the high points” about a board topic from the The American Boards of Pediatrics Pediatric Emergency Medicine Content Outline.
In this inaugural addition of PEM Core, we will review the core board content PEM physicians should know surrounding airway management and rapid sequence intubation.
To RSI or not to RSI?
Let’s start with a case.
A teenager is brought to your ED after being found unresponsive. The patient is found at a party passed out and EMS is called. EMS tells you over the phone that she is unresponsive and obtunded.
In your ED, the patient is indeed obtunded and groaning. Her GCS is less than 8. She is bradycardic and hypotensive with a respiratory rate of 8. She is gurgling and sats are around 80%. You check her airway and her jaw is clenched, but she is easy to bag with SpO2 of 80%. She has adequate pulses and perfusion.
You are worried about ingestion and but the differential is broad including trauma, metabolic issue, or sepsis. You are considering your next steps.
While knowing if there is head injury is important, this patient is not protecting her airway. Her GCS is less than 8, you hear gurgling in her airway and her jaw is clenched. Her SpO2 is only 80% with bagging– she is failing to oxygenate. This patient is in respiratory failure and the airway is not maintained, so you should not proceed with any other interventions until her airway is secure.
Though she may have other medications on board, this patient has a GCS of less than 8, is groaning and has a clentched jaw. She likely still has an airway reflex, and you will need to proceed with RSI for this intubation. Optimize her as best as you can before you initiate RSI (she is hypotensive and hypoxemic– this is a patient who should have all efforts to improve her hemodynamic parameters as she is at risk of further hypoxia and possible cardiovascular collapse!)
Noises coming from the airway should always make you nervous the patient’s airway could be compromised. A visual inspection of their airway is also important. For instance, think about a burn patient. A patient coming from a house fire, with stable vital signs and no hypoxia but has a swollen tongue, drooling and wheezing. This is very concerning for airway injury. In those cases, things are likely to get worse before they get better, and intubation is paramount before airway edema progresses.
Let's talk paralytics...
The debate surrounding use of succinylcholine or rocuronium is heated, and there are those who sit on each side of the camp. Overall, it should depend on the patient– their history, disease process, and future care.
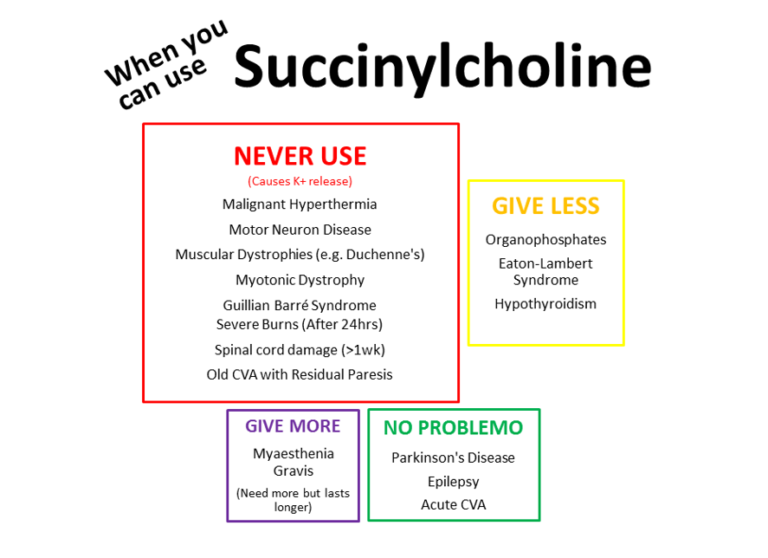
Remember that succinylcholine is a depolarizing neuromuscular blocking agent and will cause release of K+ from the cells. Therefore: When should you think about NOT using succinylcholine?
Take the infant with a history of gross motor delay who presents with respiratory failure from a respiratory infection who needs intubation. During intubation with ketamine and succinylcholine, he is then noted to have a widened QRS, which progresses to cardiac arrest.
This patient has a previously undiagnosed neuromuscular dystropy. The sudden increase in serum potassium from succinylcholine precipitated his widened QRS and subsequent cardiovascular collapse.
Dr. Laurence Boss of Oxy’s Log.
The dreaded intubation of an asthmatic
It isn’t the actual procedure of passing the tube that we dread, it is the fact that an asthmatic leads to a physiologically difficult airway with a high risk of hemodynamic collapse AND, in particular, the management of the ventilator where we can cause significant harm. If an asthmatic has progressed to respiratory failure and will need intubation, remember the patient’s pathophysiology to help you manage the ventilator settings.
- Start with a low RR (this is counter-intuitive because hyperventilation can decrease CO2)
- You’ll need a short inspiratory time and long expiratory time. Initial I:E ratio of 1:4
- Watch your pressures; keep a low PEEP and the plateau pressure <30
- Manage your sedation carefully, good sedation prevents ventilator dyssynchrony and air stacking
- Keep in mind, the transition to positive pressure ventilation will decrease a potentially already poor preload from hyperinflation of the lungs. Be prepared with fluids, pressors, and acknowledge the potential for arrest.
PEM Morsels has a great summary of mechanical ventilation for severe asthmatics.
The Great End Tidal CO2 (EtCO2)
If you haven’t seen our prior post on EtCO2, check it out! The EtCO2 can tell you a lot about a patient, and identifying classic waveforms are important content on the board exam.
See if you can identify these classic EtCO2 waveforms (all images from KI Doc Blog).
3 year old who is intubated for respiratory failure and continues to have poor saturations.
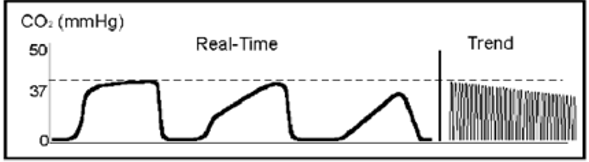
This “shark fin” appearance of the EtCO2 wave is consistent with airway obstruction, such as asthma.
You just intubated a patient and your EtCO2 looks like this.
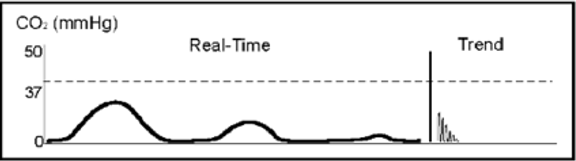
This decreasing EtCO2 immediately after an intubation indicates an esophageal intubation.
A patient with severe asthma is intubated with these waveforms.
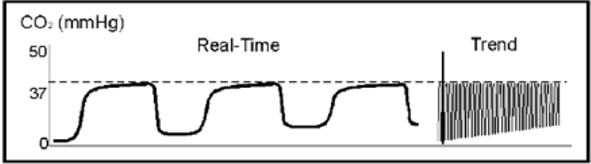
This is classic for rebreathing. This patient needs a longer expiratory time to prevent rebreathing and breath stacking.
Forty- five minutes after RSI of a patient, this is the waveform.
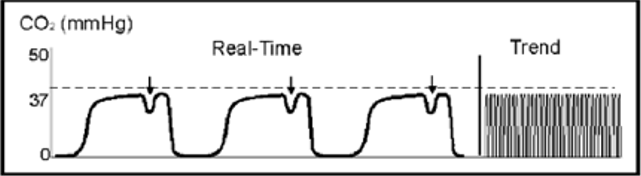
This waveform appears when muscle relaxants begin to wear off and the patient begins to breath on their own. It is called the “Curare Cleft”.
One Final Topic
You have a 2 year old who presents in respiratory failure after aspiration of a marble. The marble is visualized sitting on the vocal cords after failed ET attempt. There are multiple failed attempts to remove it, and the patient is now cyanotic with a saturation in the 40’s and HR to 60’s. BMV leads to minimal chest rise and no audible breath sounds.
You believe you need to perform a surgical airway.
The answer is all about age.
Though there is some variation, a needle cricothyrotomy is indicated for patients less than 10-12 years due to their smaller and more anterior cricothyroid membrane.
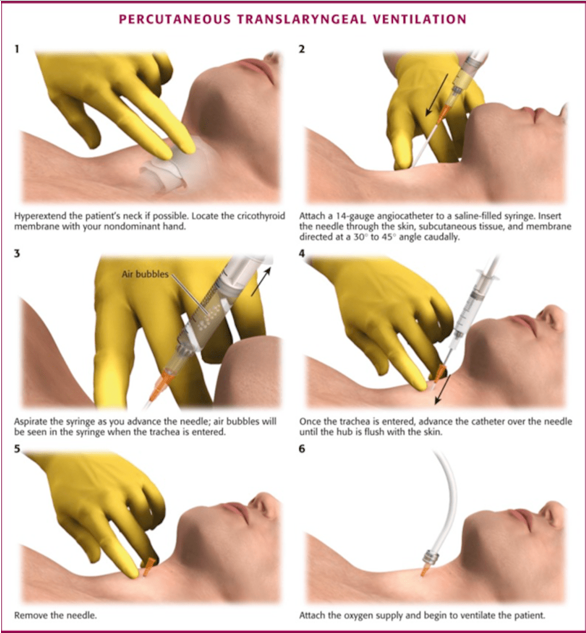
What is the procedure? Check out this great image from Brown EM Residency Blog.
References
- JMLboss (2012, April 23). OXY’s LOG- “It totally sux…”. Retrived from: https://sydneyhems.com/2012/04/23/oxys-log-it-totally-sux/
- Fox, S. (2014, November 7). Mechanical Ventilation for Severe Asthmatics. Retrieved from: https://pedemmorsels.com/mechanical-ventilation-severe-asthma/
- Leeuwenburg, Tim. (2013, November 30). So much hot gas- EtCO2 for the non-anaesthetists. Retrieved from https://kidocs.org/2013/11/much-hot-gas-etco2-non-anaesthetists/
- Ameli, Jonathan. (2015, December 9) Cricothroidotomy. Retrieved from http://blogs.brown.edu/emergency-medicine-residency/tag/cricothyroidotomy/
- Wang, V. Pediatric Emergency Medicine Question Review book 2017. Atlanta, GA. PEMQBook; 2017.


