Spine Injuries
A child comes into your trauma bay in a cervical spine collar after a fall from a 2 story window onto grass. You go through ATLS: ABC’s intact, moving all extremities, with some bruising to the right arm, leg and side of his head. Next, you evaluate the cervical spine. You carefully remove the C-collar from the screaming child and palpate the spinous processes, trying to decide if the screaming is from pain or from the 10 new faces poking and prodding the poor kid. So what do you do? Do you get a CT scan of the neck? An XRay in the trauma bay? Try to clinically clear the child?
Anecdotally, the presence of midline cervical spine tenderness and neck movement without pain in kids is often the branch point that informs the initial decision to obtain additional cervical imaging or clinically clearing the patient from c-collar. In adults, midline c-spine tenderness has a sensitivity of 86% and specificity of 43% for clinically important c-spine injuries [1]. For pediatric patients, is spinous process tenderness to palpation the most relevant exam finding to assess for clinically important spinal injuries? Let’s take a look at the evidence.
The Evidence
In a recent multicenter prospective cohort study in children, while patient reported neck pain DID reach statistical significance in regards to an association with cervical spine injury (RR 1.64, 95% CI 1.04-2.57), posterior midline tenderness to palpation DID NOT (RR 1.47, 95% CI 0.94–2.32) [2]. Similarly thoracic, lumbar, and sacral spine tenderness were also not associated with clinically important spine injuries. Leonard et al. DID find some additional factors that were associated:
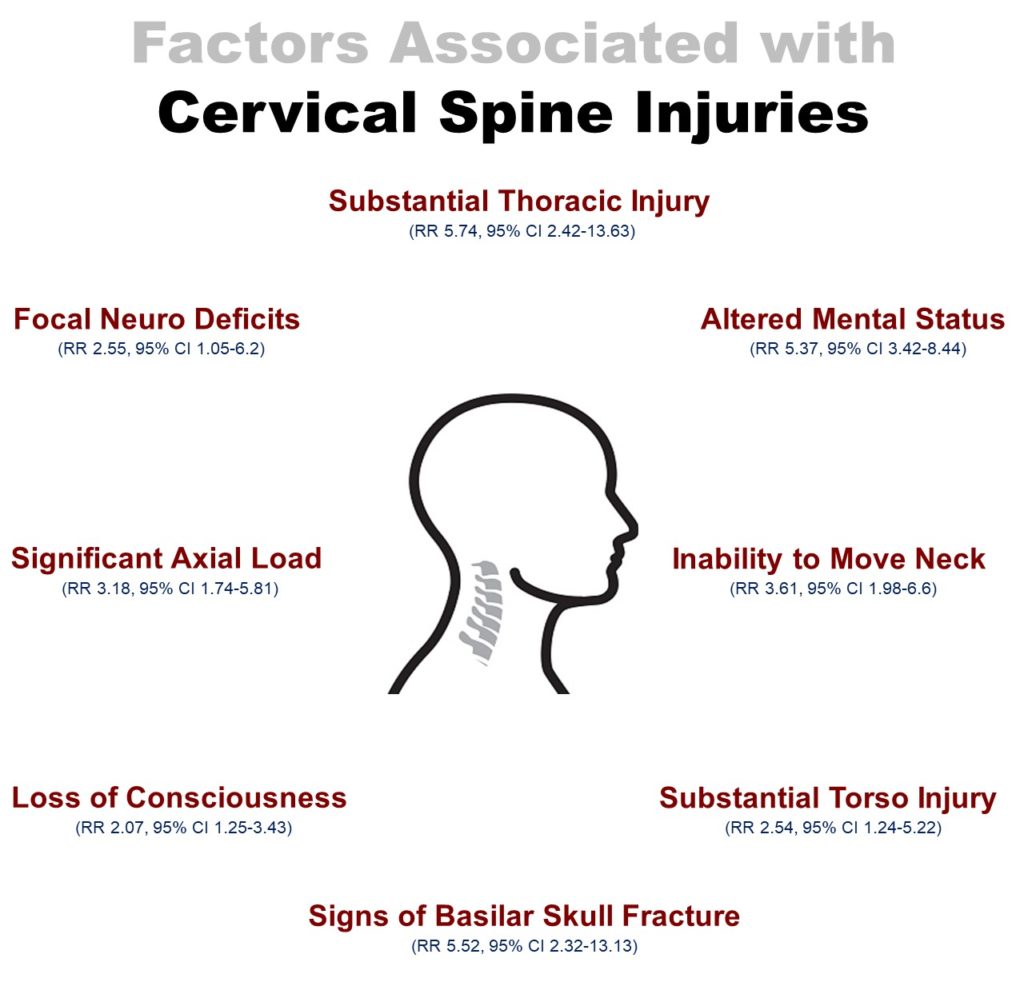
Adapted from Leonard JC, Browne LR, Ahmad FA, et al. Cervical Spine Injury Risk Factors in Children With Blunt Trauma. Pediatrics 2019;144.
Put simply, if a patient has midline cervical tenderness to palpation, they likely need imaging to assess for injury. However it is important to know that the lack of midline cervical tenderness does NOT exclude risk for injury, and factors such as the ones above have shown stronger associations with cervical spine injuries.
The Cervical Spine: To Scan or Not to Scan...
That really is the question. Cervical spine injuries are uncommon in children (1.8% of cases in children in which cervical imaging obtained) [2]. As such, providers are often thoughtful in choosing the right imaging modality to reduce radiation exposure. A common practice we see at our institution is ordering cervical spine x-rays as the initial imaging modality, although the patient may already be undergoing CT scans of other potential areas of injury (i.e. head, chest, abdomen/pelvis). CT is much more sensitive than X-ray at detecting cervical spine injuries, but plain radiographs can be appropriate initial tests especially in low-risk patients [3]. This brings us to another important question– what is the most appropriate location to obtain cervical spine x-rays (i.e. portable XR in the trauma bay vs after being transported to radiology)? Some providers strongly advocate for obtaining cervical spine radiographs in the trauma bay, the benefit being earlier diagnosis of important spine injury and can help providers determine the need for a subsequent CT scan. This can also limit the amount of transport back and forth to radiology, which can be beneficial especially is there is concern for an unstable fracture.
What about an MRI?
If there is concern for a neurologic deficit secondary to cord injury, edema or hemorrhage, MRI is indicated.
Stable as a table or unstable as a...um...wobbly chair...
In first step in delineating spinal fracture stability is to understand the three-column concept (Denis Classification).
The Anterior Column
Made up of the anterior 1/2 of the vertebral body/disc/annulus and the anterior longitudinal ligament.
The Middle Column
Made up of the posterior 1/2 of the vertebral body/disc/annulus and the posterior longitudinal ligament.
The Posterior Column
Made up of the facet joints, the transverse process, and the ligamentum flavum.
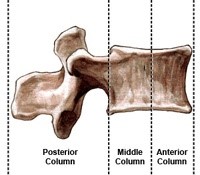
Stability of the fracture is based on which and how many of these columns are involved. If the fracture involves the anterior column-only, it is stable. If the fracture involves the anterior+middle column, or the anterior+middle+posterior column they are considered unstable .

1. Posterior midline cervical tenderness does not effectively rule in or rule out cervical spine injury.
Cervical tenderness on exam should be taken into context with other clinical factors such as mechanism, injury pattern, inability to move neck, altered mental status and neurologic deficits.
2. Consider ordering portable cervical spine x-rays, which can be a good initial imaging modality in low risk patients, in the right clinical context.
3. If there is a neurologic deficit, obtain a stat MRI
4. Stability of the fracture is based on the number of columns involved.
Additional FOAMed:
References:
1. Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001;286:1841-8.
2. Leonard JC, Browne LR, Ahmad FA, et al. Cervical Spine Injury Risk Factors in Children With Blunt Trauma. Pediatrics 2019;144.
3. Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma 2005;58:902-5.
4. Highsmith, J. Types of Spinal Fractures. Retrieved from: https://www.spineuniverse.com/conditions/spinal-fractures/types-spinal-fractures

Preston Dean is a current pediatric emergency medicine fellow interested in resuscitation/critical procedures and respiratory tract infections.




