PEM/Radiology Conference with Dr. Stratton and Dr. Jones
Case: A school-aged boy with right afferent pupil defect and gait instability.
Let’s go back to basics:
What the heck is an Afferent Pupillary Defect (APD) aka a “Marcus Gunn Pupil” (who, by the way, was a Scottish Ophthalmologist who got to name the finding in the 1800s)?
When the light hits the affected eye, that pupil will constrict only slightly. Light into the non-affected eye will cause brisk constriction of the pupil. It is discovered by performing the swinging light test whereby you swing the flashlight to left eye and right eye – see video below. If you have an abnormal swinging light test you should be thinking of optic nerve disorders, but in particular optic neuritis.
Video by U-M Kellogg Eye Center in Ann Arbor (Link)
Diagnosis?
Optic neuritis
Optic Neuritis is caused by damage to the optic nerve secondary to inflammation. It commonly presents to the emergency department as: [1]
- Vision loss
- Afferent pupillary defect (see above)
- Optic disc swelling and papilledema
- Decreased perception in red colors
- Decreased visual acuity
- Eye pain
- Retro-orbital headache
An important consideration for pediatrics is that it commonly presents as Bilateral optic neuritis and it usually follows a viral infection [2]
it is best to break down the differential diagnosis for optic neuritis into three categories.
- Demyelinating Lesions:
- Neuromyelitis Optica (see below)
- Multiple Sclerosis
- Schilder’s disease
- Autoimmune:
- SLE
- Sarcoidosis
- Post-viral syndromes
- Infectious:
- Herpes
- Lyme
- Syphilis
A note about Neuromyelitis Optica (aka NMO ): It is a demyelinating disease that preferentially affects optic nerves and spinal cords. The condition is a spectrum that has expands to include unilateral optic neuritis, brainstem, cerebral, and diencephalic syndrome. An MRI is the image of choice but not necessary for diagnosis. Diagnosis can be made through history and ophthalmologic exam. [3]
Case: Adolescent female with headache, intermittent symptoms of double vision, right-sided weakness and numbness with word-finding difficulty
Let’s go back to basics:
From an ED perspective, what is the FIRST thing that needs to be ruled out?
Stroke!
Why we do what we do for acute stroke imaging:
- The Non-Contrast CT Scan
The question to be answered: Blood or not?
Utilized to make the first decision point regarding thrombolytic therapy - The CTA or MRI/MRA
The question to be answered: Is there a thrombus?
Utilized to make decisions about a target for thrombectomy - Perfusion imaging
The question to be answered: how much brain is affected?
Shows area of perfusion deficits
Utilized for its predictive value and risk/benefit decision making– Not quite integrated into the pediatric world
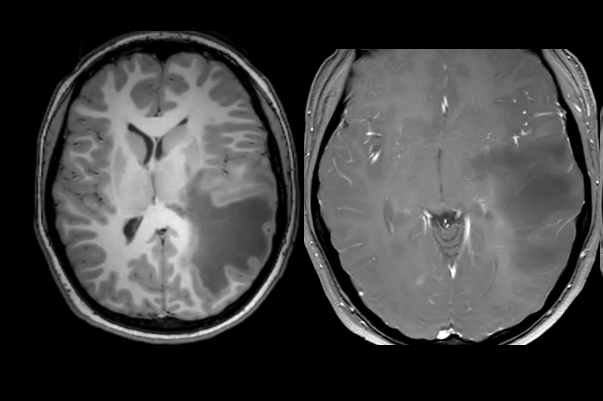
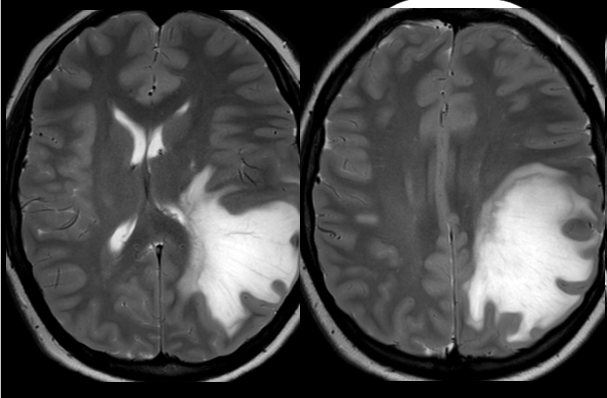
A MRI was obtained and showed a large mass effect causing lesion with significant surrounding edema. Photo courtesy of Dr. Blaise Jones
Diagnosis?
Multiple Sclerosis (MS)
What is Multiple Sclerosis (MS)?
- MS is a progressive, replasing/remitting chronic inflammatory autoimmune disease affecting the central nervous system
Pediatric MS is when symptoms occur before the age of 16.
What are the presenting symptoms in kids? [4]
- Optic neuritis
- Sensory symptoms (paresthesias)
- Motor symptoms (fatigue, weakness, diplopia)
- Brainstem symptoms (ataxia, transverse myelitis)
- Kids tend to have a polyfocal onset and more frequent relapses [5]
Pediatric MS is often confused with Acute disseminated encephalomyelitis (ADEM) and encephalitis
Be suspicious in the pediatric patient with multiple episodes of odd neurologic symptoms.
MRI imaging is important in making the diagnosis of MS.
Tumefactive Multiple Sclerosis (Demyelinating lesions)(above image)
Tumefactive demyelinating lesions are large space-occupying lesions that can mimic tumors. These can be seen in patients with MS.
Sanchez et al. did a study looking at tumefactive demyelinating lesions in 15 patients diagnosed with MS [7]
- ~2% of MS cases
- Mean age 36yo
- 4 out of 5 converted to MS by 8mo
- Common radiologic findings
- 2 out of 3 solitary lesions were primarily in the frontal or parietal lobe
- Open-ring enhancement
- A large demyelinating lesion can cause enough edema to lead to a mass effect in the brain.
- Treatment: steroids, plasma exchange. Rituximab, cyclophosphamide
Case: A young adult with a thunderclap headache after intercourse, now resolved.
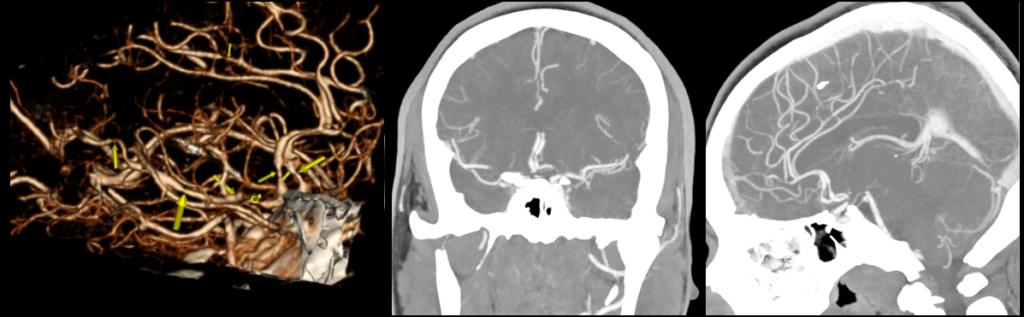
A perfusion study was obtained and showed multiple areas of vasoconstriction in the cerebral arteries shown by the yellow arrows. Photo courtesy of Dr. Blaise Jones
Diagnosis?
Reversible Cerebral Vasospasm Spectrum/Syndrome (above image)
What is it?
- Syndrome defined by:
- Recurrent thunderclap HA- with or without associated neurologic symptoms
- Reversible vasoconstriction of at least 2 different cerebral arteries
What causes it?
- Disturbances of the cerebral vascular tone, exposure to vasoactive drugs, or the peripartum period are associated with it.
- Generally occurs once in a person’s life (though with an average of 4 attacks of pain during that one occurrence) and then resolves within a 12 week period. To be aware: though “reversible” is in the name, there are less than 5% of cases that have progressive vasoconstriction leading to stroke [6]
This syndrome encompasses many other described phenomena including Call-Flemming, postpartum angiopathy, migrainous vasospasm or migraine angiitis, drug-induced cerebral arteritis or angiopathy, sexual HA.
- Chukwulebe S, Gappmaier V. (2019, March 11). Optic Neuritis. [NUEM Blog. Expert Commentary by Simon S]. Retrieved from http://www.nuemblog.com/blog/optic-neuritis
- Pérez-Cambrodí RJ, Gómez-Hurtado Cubillana A, Merino-Suárez ML, Piñero-Llorens DP, Laria-Ochaita C.Optic neuritis in pediatric population: A review in current tendencies of diagnosis and management. J Optom. 2014 Jul; 7(3): 125–130.
- Germann CA, Baumann MR, Hamzavi S. Ophthalmic diagnoses in the ED: optic neuritis. Am J Emerg Med. 2007;25(7):834-7.
- Fox, S. (2017, Sep 7). Multiple Sclerosis in Children. Retrieved from https://pedemmorsels.com/multiple-sclerosis-in-children/
- Alroughani R1, Boyko A2. Pediatric multiple sclerosis: a review. BMC Neurol. 2018 Mar 9;18(1):27. PMID: 29523094.
- Mehdi, A. & Hajj-Ali, R.A. Curr Pain Headache Rep (2014) 18: 443. https://doi.org/10.1007/s11916-014-0443-2
- Sánchez P, Meca-Lallana V, Barbosa A, Manzanares R, Palmí I, Vivancos J. Tumefactive demyelinating lesions of 15 patients: Clinico-radiological features, management and review of the literature. J Neurol Sci. 2017 Oct 15;381:32-38. doi: 10.1016/j.jns.2017.08.005. Epub 2017 Aug 12.

Ashish Shah is an assistant professor and Pediatrics and Family Medicine Residency Education Director at Rady Children’s Hospital interested in creating PEM 4 all stages of learners caring for children seen in the emergency department

Katie Edmunds is a current Pediatric Emergency Medicine Fellow interested in creating PEM 4 all those who are given the responsibility of treating the sickest babies wherever they may be.



